11 Essentials for Accurate Pulse Oximeter Readings
Pulse oximeters are small, handy tools that show blood oxygen saturation (SpO2) and pulse rate. People use them at home to watch lung or heart conditions and to spot changes early. This guide explains what readings usually mean, why numbers sometimes shift, and how to get reliable results. You’ll find clear thresholds for concern and practical steps to fix common errors. I’ll also point out the difference between consumer fingertip models and the more precise hospital probes. Where numerical claims appear, they come from reputable sources such as peer-reviewed research, professional associations, and respected consumer health outlets — see inline notes. This article favors straightforward steps you can try at home: keep your hand warm, place the probe correctly, wait for a steady value, and look at trends rather than single numbers. If you care for older relatives or people with chronic lung conditions, these checks can reduce worry and help you decide when to call a clinician. As a quick cultural note for readers who may also use similar devices in different contexts, a simple practice like keeping a small cloth near the tiffin box to warm cold fingers before reading can make a measurable difference. Read through the eleven essentials below, use the practical checklists, and keep the device manual handy for model-specific advice.
1. What a "normal" SpO2 looks like at rest (95–100%)

SpO2 stands for peripheral oxygen saturation and reflects the percentage of oxygenated hemoglobin in the blood. For most adults at rest, a normal SpO2 range is between 95% and 100%. Readings that stay below 92% are considered concerning and should prompt consultation with a healthcare provider. If values fall to 88% or lower, urgent evaluation is recommended. (Sources: Verywell Health; clinical guidelines.) These thresholds are general; some people with chronic lung disease, such as COPD, may have lower baseline numbers that their doctor has already discussed. Altitude can also lower normal readings slightly, so expect modest variation if you live or travel at high elevation. For home users, record a few readings while relaxed and breathing normally to establish a personal baseline. If you care for an older family member or a child, note that children typically have similar resting ranges, but clinical context matters. Keep a log with time of day, activity level, and any symptoms like breathlessness or chest tightness. That record helps clinicians judge whether a low reading is an isolated blip or part of a trend that needs attention.
2. Why pulse oximeters have an accuracy range (±3% typical)

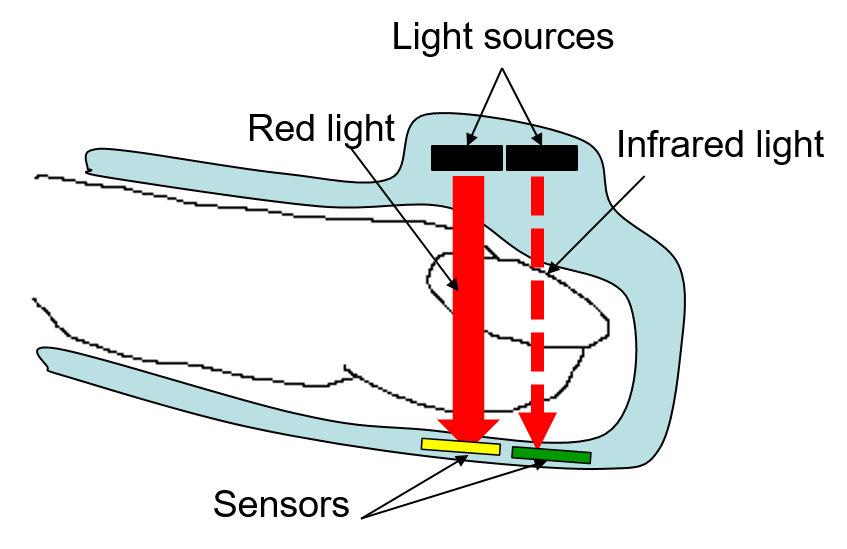
Pulse oximeters estimate oxygen saturation by measuring how red and infrared light passes through tissue and blood. This indirect method works well but has limits; under ideal conditions, many devices report accuracy around plus-or-minus three percentage points. Laboratory and clinical studies support a typical accuracy range of ±3% in stable conditions. (Source: PMC/NIH research.) Consumer fingertip units may perform slightly differently from hospital-grade probes, and manufacturing differences explain some variability. Real-world conditions like motion, low perfusion, and skin pigmentation can widen the practical error range, so a 95% reading might actually be 92% or 98% depending on circumstances. For critical clinical decisions, top-tier hospital monitors with validated probes are preferred because they undergo stricter testing and calibration. For home monitoring, the important takeaway is to understand the built-in uncertainty and use the device to watch trends and symptoms, rather than treating one isolated number as definitive. When exactness matters, clinicians rely on arterial blood gas testing rather than pulse oximetry.
3. Fingertip devices vs clinical probes: what differs

Consumer fingertip oximeters are compact and convenient for quick checks at home. Clinical probes, used in hospitals, often have more robust sensors, better signal processing, and tighter accuracy specifications. Hospital probes are designed for continuous monitoring and are tested against strict standards, while many home models are optimized for cost and portability. The result is that clinical equipment usually gives more consistent readings under challenging conditions like movement or low perfusion. For most healthy people, a reliable fingertip unit will suffice for routine checks, but caregivers should be aware of the distinction when a health emergency requires precise measurement. If a home reading is unexpectedly low, a clinic-grade device or an arterial blood gas measurement can confirm the result. Some higher-end consumer models advertise advanced algorithms that reduce motion artifacts; check independent reviews and look for devices with FDA clearance or similar regulatory marks. Keep in mind that probe placement and maintenance are important for both types; a well-used clinical probe can outperform a poorly used higher-end fingertip model.
4. How skin tone can affect readings and what to do

Research has shown that optical pulse oximeters can be less accurate for people with darker skin tones, especially at lower oxygen saturations. Some studies and manufacturer reports note a tendency toward overestimation in certain situations, meaning low saturations could be missed. (Source: Medtronic research; recent studies.) The practical response is simple and respectful: if a low reading is unexpected, verify it using a second finger, try a different device, and assess symptoms like breathlessness, color changes, or altered mental state. Clinicians should be aware of this limitation and not rely solely on a single pulse oximeter value when evaluating people with darker skin. At home, getting a baseline when healthy helps spot real changes later. If you wear a device for the whole family, note which readings have matched clinic values historically; that helps you know which device and method are most reliable for your household. In clinical settings, teams increasingly pair pulse oximetry with other measures such as respiratory rate and clinical exam to reduce bias in decision-making.
5. Why movement, cold fingers, and poor perfusion matter

Pulse oximeters rely on a steady pulse and good blood flow under the sensor. Movement blurs the optical signal; cold fingers reduce blood flow and make readings unstable. Poor perfusion from low blood pressure, vasoconstriction, or peripheral vascular disease can also cause erratic or falsely low values. To improve reliability, warm the hand, sit quietly, and support the arm at heart level before taking a reading. Wiggle-free stillness for 30 to 60 seconds often yields a stable number. If perfusion remains low, try another finger or the earlobe, which sometimes has better blood flow. For people who work outdoors or in cold environments, carrying a small hand warmer or rubbing the hands briefly can help. In clinical practice, monitors may use signal-quality indicators to warn when the reading is unreliable; many consumer devices lack such features, so the user must judge stability by watching the display and pulse waveform where available.
6. Nail polish, artificial nails, and how to avoid errors

Dark nail polish and acrylic or artificial nails can block the light path and distort readings. The simplest fix is to remove polish from the finger you plan to use or choose an alternate finger without polish. If that is not possible, use the earlobe or another site that the probe can access. When caring for elders who often have painted nails or long nails, keep a small buffer or nail remover in the first-aid kit so a quick check doesn’t become a guessing game. Artificial nails can be lifted slightly near the nail plate to allow light through if removal isn’t feasible, but removal is preferable. Also, ensure the sensor does not press too tightly and that the finger is free of lotion or dirt that could scatter light. These steps reduce a common source of false low or unstable readings and are easy to apply before a check.
7. Correct finger placement and how long to wait for a stable reading
Place the probe on a clean middle or index finger and ensure the sensor covers the entire fingertip. The finger should sit comfortably and not be crushed by the clip. Hold the hand relaxed and supported at heart level while the device measures. Many users glance too soon; wait at least 30 seconds for the display to stabilize and consider 60 seconds for the most reliable value, especially if readings fluctuate. If the device shows a pulse rate that matches your expectation and remains steady, the SpO2 number is more trustworthy. If the pulse reading is erratic or absent, reposition the finger and try again. Keep the hand warm, and remove rings if they pinch the finger. For caregivers checking multiple people, adopt a consistent routine for finger choice and wait time; consistency reduces random variation across readings and makes trends easier to interpret.
8. Why trends matter more than single readings

A single SpO2 reading is a snapshot and can be affected by temporary factors. Monitoring trends over hours or days gives a clearer picture of respiratory function. For example, a drop from a usual 97% to 94% over several checks may be more meaningful than an isolated 93% that quickly returns to baseline. Keep a simple log with time, activity, and symptoms to track changes. Many smart devices and apps can record values automatically; these tools make it easier to share trends with clinicians. When you see a sustained downward pattern or increasing variability, contact a healthcare professional. Trend-based monitoring is especially useful for people with chronic conditions or those recovering from respiratory illness; it helps catch gradual deterioration earlier than one-off checks would. If possible, include pulse rate and notes about breathing effort alongside SpO2 numbers to give clinicians more context.
9. Home monitoring vs hospital monitoring: different expectations

Hospital monitors are designed for continuous, precise monitoring and are judged by stricter performance and calibration standards. Home pulse oximeters are made for spot checks and trend watching, not for making complex treatment decisions alone. Expect hospital equipment to perform better in conditions like motion or low perfusion because of advanced sensors and software. At home, use your device for routine checks, early-warning signs, and to follow a clinician’s instructions. If a clinician needs exact saturation levels for treatment decisions, they may repeat readings with clinical equipment or order arterial blood gas testing. That said, home monitoring has clear value: it empowers patients, helps with timely communication, and can reduce unnecessary clinic visits. When sharing home readings with a clinician, be honest about the device type and any factors that might affect accuracy, such as cold hands or nail polish.
10. When low readings require medical attention (thresholds)

Use thresholds as guides rather than absolute rules. In general, persistent SpO2 below 92% should prompt medical consultation. Readings at or below 88% are commonly treated as urgent and may require emergency evaluation. (Source: Verywell Health; clinical practice references.) Always consider symptoms alongside numbers: breathlessness, chest pain, confusion, or fainting with a low reading is an emergency. A single low reading that corrects quickly after warming the hand or resting is less alarming than a sustained decline. If in doubt, call your clinician or local emergency services and report the trend and symptoms, not just one isolated number. For people with doctor-defined target ranges, follow those targets. Caregivers responsible for older adults or people with chronic lung disease should have an action plan that specifies when to seek care based on baseline values and symptom changes.
11. Choosing, maintaining, and validating your device

Buy a pulse oximeter from reputable brands with positive independent reviews and regulatory clearances when possible. Look for FDA clearance or similar certifications to ensure basic performance standards. Read the manual for recommended cleaning steps and avoid harsh solvents that can damage sensors. Replace batteries as directed and store the device in a dry place away from extreme temperatures. Periodically validate your home device against clinic-grade equipment if you have the chance; many clinics will compare readings during a visit. Keep a backup unit if monitoring a high-risk person to avoid gaps if a device fails. Finally, check sensor integrity regularly: loose clips, worn LEDs, or cracked casing can degrade accuracy. Proper care and occasional cross-checks will keep your device useful for reliable home monitoring.
Final thoughts: Use pulse oximetry wisely

Pulse oximeters are helpful tools when used with an understanding of their limits. They give quick insight into oxygenation and can flag changes that need attention, but no device replaces clinical judgment. Get to know your device: find a finger that gives steady readings, warm or cold hands first, avoid nail polish or artificial nails on the measuring finger, and wait for the value to stabilize. Track trends rather than reacting to a single low number, and keep a simple log of readings with symptom notes to share with clinicians. Be mindful that factors such as skin tone, motion, and poor perfusion can change results; when readings conflict with how someone looks or feels, trust symptoms and seek verification. Keep the device in good working order by following manufacturer care steps, replacing batteries, and validating against clinic equipment when you can. If a sustained reading stays below your doctor’s threshold — often 92% or lower — or if there are alarming symptoms like severe breathlessness or chest pain, get urgent medical help. Used thoughtfully, a pulse oximeter is a practical ally for home monitoring and can support better conversations with healthcare professionals.
